As part of our series spotlighting STI’s, this month we’re looking at genital warts.
Sexually transmitted infections (STIs) are an infection that can be passed on between sexual partners during unprotected sexual contact. There are more than 25 STIs which can be spread by vaginal, anal or oral sex.
They are unfortunately common amongst all age groups, which is why it’s important to understand what they are, the symptoms you may experience and how they are .
It’s important to start breaking the stigma surrounding STIs by showing that they aren’t something to be embarrassed about and, in most cases, can be very simple and quick to get treated.
So, let’s have a look at what genital warts is and what you need to know about it.
What are Genital Warts?
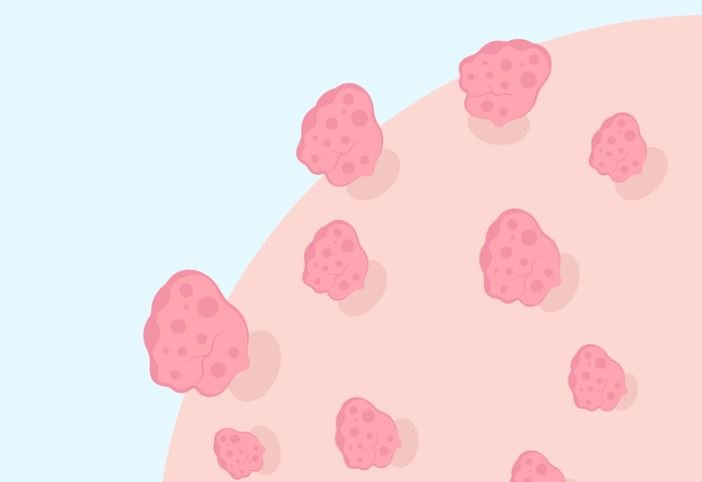
Genital warts are small growths or lumps that appear on the genital or anal areas. They are caused by certain strains of HPV, a virus that is transmitted through intimate skin-to-skin contact. While many strains of HPV exist, only a few are responsible for genital warts.
Transmission
HPV is highly contagious and can be spread through vaginal, anal, and oral sex. It can also be transmitted through close genital contact without penetration. Using condoms can reduce the risk of transmission but may not completely prevent it, as warts can be present on areas not covered by a condom.
Symptoms
Genital warts often appear as small, flesh-coloured bumps or groups of bumps in the genital area. They can be smooth or have a cauliflower-like appearance. Some individuals may experience itching, discomfort, or bleeding with warts, though they are typically painless. Warts can appear weeks or even months after exposure to HPV, making it difficult to trace the source of infection.
Diagnosis
Diagnosis is usually made through a visual examination by a healthcare provider. In some cases, a biopsy may be taken to confirm the presence of HPV. Regular sexual health check-ups are crucial, especially for those with new or multiple partners. Suffolk Sexual Health Services can point you in the right direction as to where to get a biopsy.
Treatment Options
While there is no cure for HPV, treatments can remove visible warts. Options include:
- Topical Treatments: Creams and ointments prescribed by a healthcare provider can be applied directly to the warts.
- Cryotherapy: Freezing the warts with liquid nitrogen.
- Electrocautery: Burning off warts using an electric current. Although Suffolk Sexual Health Services do not provide this has a treatment choice, we can direct you to the right place.
- Surgical Removal: In some cases, warts may need to be surgically removed.
It is important to note that while these treatments can remove warts, they do not eradicate the virus from the body. Warts may recur, and regular monitoring and follow-up treatments may be necessary.
Prevention
Preventing genital warts involves reducing the risk of HPV transmission:
- Vaccination: The HPV vaccine is highly effective in preventing infections with the strains of HPV most associated with genital warts and cervical cancer. It is recommended for preteens but can be given up to age 26, and in some cases, up to age 45. Please ask your GP about this.
- Condom Use: Consistent and correct use of condoms can lower the risk of HPV transmission, though it is not 100% effective. To get FREE condoms, please check out our eC-Card scheme here.
- Regular Screening: Regular sexual health screenings and Pap smears for women can help detect HPV-related changes early, allowing for timely management. To order a FREE STI test kit, please click here.
Living with Genital Warts
Having genital warts can be emotionally and physically challenging. It is important to communicate openly with sexual partners and seek support from healthcare providers. While the presence of genital warts can be distressing, most cases do not lead to serious health problems, and the immune system often clears the virus over time.
Conclusion
Genital warts are a common STI caused by HPV. Awareness, vaccination, and safe sexual practices are key to prevention and management. If you suspect you have genital warts or have been exposed to HPV, seek medical advice for appropriate testing and treatment options.
For more detailed information, visit the Suffolk Sexual Health Service.